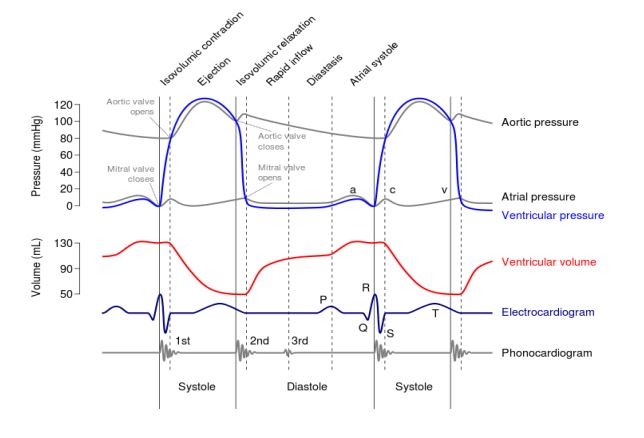
Describe in detail with diagram of Events in cardiac cycle.
Definition: The cyclical changes that take place in the heart during each beat (one systole and
one diastole)
Duration for one cycle = 0.8 sec
Phases:
- Atrial systole -0.1 sec
- Atrial diastole- 0.7 sec
- Ventricular systole – 0.3 sec
- Ventricular diastole – 0.5 sec
#ATRIAL SYSTOLE
- Contraction of atria & expulsion of blood into ventricles
- Contributes 25% of the ventricular filling
- Last phase of ventricular diastole
- Produces fourth heart sound
#ATRIAL DIASTOLE
- Gradual filling of atria by blood brought by veins
#VENTRICULAR SYSTOLE
- Contraction of ventricles & expulsion of blood into respective blood vessels
Includes three phases
Isovolumetric contraction-0.05sec
Maximal ejection – 0.1 sec
Reduced ejection – 0.15 sec
Isovolumetric contraction
- Period between closure of AV valves & opening of semilunar valves
- Ventricles contract as closed chambers
- No change in the volume of blood in the ventricles
- Intraventricular pressure increases
Maximal Ejection phase
- Increase in intraventricular pressure
- Semilunar valves are forced to open
- Due to High Pressure gradient, blood is rapidly ejected out of ventricles
- About 2/3rd of stroke volume is ejected
Reduced ejection
- Due to decreased pressure gradient, the rate of ejection of blood is reduced
- About 1/3rd of stroke volume is ejected
#VENTRICULAR DIASTOLE
- Filling of ventricles by the blood flowing from atria
- Includes five phases
Protodiastolic period – 0.04 Sec
Isovolumetric relaxation – 0.08 Sec
Rapid inflow – 0.11
Diastasis – 0.19
Atrial systole – 0.11
Protodiastolic phase
- Ventricle relaxes
- Intraventricular pressure in less than the pressure in the aorta/Pulmonary Arteries
- Semilunar valves close to prevent the back flow of blood from arteries into ventricles
- Closure of SLV produces second heart sound
Isovolumetric relaxation
- Period between closure of semilunar valves & opening of AV valves
- SLV and AV valves are closed
- Ventricle relaxes as closed chamber
- No change in the volume of blood in the ventricles
- Intraventricular pressure decreases
Rapid inflow phase
- Intraventricular pressure less than intra atrial pressure
- Hence AV valves open
- Blood flows from atria to ventricle at a faster rate
- Turbulence due to rapid flow produces third heart sound
Diastasis
- Increase in intraventricular pressure
- Blood flow from atria to ventricle at low rate or static
Atrial systole
- Last phase of ventricular diastole
- Contributes additional 25% of ventricular filling
Define cardiac output. Discuss the factors regulating cardiac output.
A) Definition:
- Cardiac output (CO) – Volume of blood ejected by each ventricle / minute
- Stroke volume (SV) – Volume of blood ejected by each ventricle / beat
- Cardiac Index (CI) – Cardiac output / square meter of the body surface Area
- End Diastolic Volume (EDV) – Volume of the blood in the ventricle at the end of diastole
- Ejection Fraction (EF) – Fraction of the end diastolic volume that is ejected
- Peripheral Resistance (PR) – The resistance offered to the blood flow in the peripheral blood vessels
B) Normal values:
- Cardiac output – 5 lts / min
- Stroke volume – 70 ml/ beat
- Cardiac index – 3 lts/ min/square metre of body surface area
- End diastolic volume – 120 ml
- Ejection Fraction — 65%
METHODS TO DETERMINE CARDIAC OUTPUT
Direct method
Indirect method
➢ Fick principle
➢ Dilution principle (Dye. Isotope & Thermo dilution)
➢ Ballistocardiography
➢ Pulse pressure contour
➢ X – ray cardiometry
FICK PRINCIPLE
The cardiac output is calculated by the following formula
X
Q = ———-
A – V difference
Q – Blood flow
X – Amount of substance taken up by an organ
A — V difference = Arterio venous difference in the concentration of a substance
As pulmonary blood flow is equal to cardiac output, pulmonary blood flow determined by Fick principle is taken as cardiac output.
Pulmonary blood flow = amount of O2 taken by the lungs/minute
————————————————–
Arterio venous difference of O2
For example
Amount of oxygen taken by lungs / minute = 250 ml
(Determined by spirometer)
Arterial oxygen content = 20 ml / 100 ml of blood
(Estimated from any peripheral artery)
Venous oxygen content = 15 ml / 100 ml of blood
(Estimated from right atrium)
Pulmonary blood flow = 250
– ——– X 100 = 5000 ml 0r 5 lts
20 – 15
As pulmonary blood flow = cardiac output, CO = 5 lts
Describe the factors regulating cardiac output?
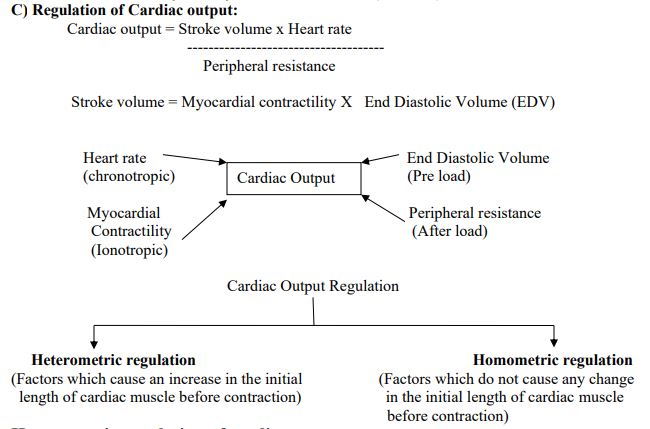
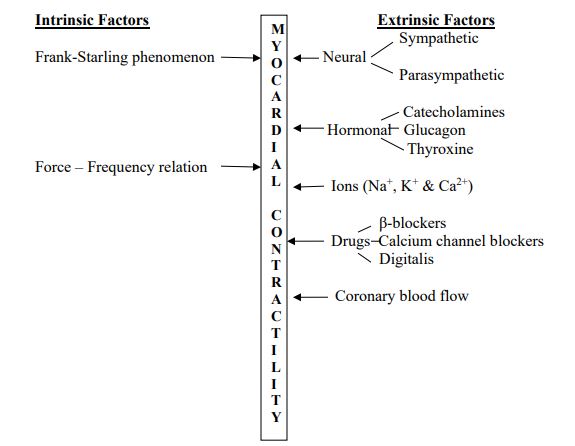
Heterometric regulation of cardiac output
I. Intrinsic factors regulating myocardial contractility
Frank – Starling Phenomenon:
The force of contraction is directly proportional to the initial length of the
cardiac muscle. The initial length of the muscle depends on the end diastolic
volume. Any increase in the EDV stretches the ventricular myocardium,
increasing the length of the muscle fiber
Importance:
- – helps to match the stroke volume of the ventricles
- – helps to maintain the minute output
- – prevents venous engorgement
Force Frequency relation:
Any increase in the frequency of heart beat increases myocardial contractility within physiological limits. The increase in contractility is due to accumulation of intracellular calcium ions
II. End Diastolic volume:
End Diastolic Volume (EDV) is the volume of blood in the ventricles at the end of diastole. Any increase in the EDV increases the cardiac output by increasing the stroke volume.
Mechanism: Increase in EDV → stretching of ventricular muscle fibres →Increase in the length of fibres → stronger muscle contraction
→Increase in cardiac output (Frank Starling’s law)
Factors influencing EDV:
i) Venous return
ii) Ventricular compliance
iii) Diastolic pause
iv) Atrial systole
Venous return: The volume of blood that returns to the atria through the veins in one minute. This increases EDV & there by increases cardiac output.
Factors influencing venous return:
1. Cardiac pump: The pumping action of ventricles increases venous return by 2 forces:
❖ Vis – a – tergo (propelling force from behind):
– Left ventricular contraction during systole and elastic recoiling of arteries during diastole push the blood from aorta towards the right atrium
❖ Vis – a –fronte (suction force from front) – Right atrial pressure:
– Less pressure in right atrium during diastole helps in suction of blood from the great veins into the right atrium
2. Capacity of venous reservoir: This factor is inversely proportional to venous return .
Venoconstriction → decrease in venous capacity → increase in venous return
3. Blood Volume: Directly proportional to venous return.
e.g., hemorrhage → decrease in blood volume → decrease in venous return
4. Respiratory pump: Venous return increases during inspiration
Inspiration → negative intrathoracic pressure → suction of blood into thoracic big veins → increased venous return
5. Muscle pump: Intermittent contractions of skeletal muscle particularly leg muscle → squeeze the veins → increases the flow of venous blood towards the heart → increase in venous return
6. Abdominal pump: Contractions of abdominal muscles →compresses the great veins, pushing venous blood towards the heart

Ventricular compliance:
– refers to the stretchability of ventricular myocardium
– any increase in the compliance reduces EDV and thereby stroke volume
e.g constrictive pericarditis & pericardial effusion
Diastolic pause:
- – refers to the duration of diastole of ventricles
- – this influences the ventricular filling
- – this factor is directly related to EDV within physiological limits
Atrial systole:
- – contributes 20% of ventricular filling at rest
- – influences EDV directly
e.g
- – increase in atrial systole during exercise → increase in EDV
- – in atrial flutter & fibrillation, the contribution of atrial systole in ventricular filling is reduced
Homometric Regulation of Cardiac Output
I . Extrinsic Factors Regulating Myocardial Contractility
a) Neural factors:
Sympathetic stimulation: Releases nor-epinephrine → binds to β1 receptors → increases
cAMP → increase in intracellular calcium → increase in myocardial contractility
Parasympathetic stimulation: Releases acetylcholine → binds to muscarinic receptors
(M2) → hyperpolarization of SA nodal and myocardial cells → decrease in myocardial contractility
b) Hormones:
Epinephrine & Nor-epinephrine: Bind to β1 receptors →increase in cAMP → increase in intracellular calcium → increase in myocardial contractility
Glucagon: Increases myocardial contractility by increasing intracellular calcium without binding to β1 receptors
Thyroxine: Increases the myocardial contractility by increasing the metabolic rate.
c) Ions:
Sodium & Potassium – decreases the myocardial contractility
Calcium – increases the myocardial contractility
d) Drugs:
β – blockers: e.g Propanaolol – block the β – receptors and decreases the myocardial contractility
Calcium-channel blocker: e.g Verapramill – block the calcium channel → decrease in intracellular calcium → decrease in myocardial contractility
Digitalis: Blocks Na+ – K + ATPase → decrease in Na+ gradient across the membrane → calcium accumulation inside the cell → increase in myocardial contractility
e) Coronary blood flow:
Decrease in coronary blood flow
↓
Hypoxia, hypercapnia & acidosis
↓
Decrease in myocardial contractility
Influence of heart rate on cardiac output
Direct relationship between heart rate and cardiac output
Increase in HR
↓
Increase in intracellular calcium
↓
Increase in force of contraction
– This happens by two ways:
1. As a multiplying factor
2. Staircase phenomenon
(This relation is linear upto 180 BPM. Beyond this level, venous return falls → decrease in cardiac output)
Influence of peripheral resistance on cardiac output:
– Initially, the variation in peripheral resistance tends to influence cardiac output
– But the indirect effects maintain the cardiac output
———————————————————————————–
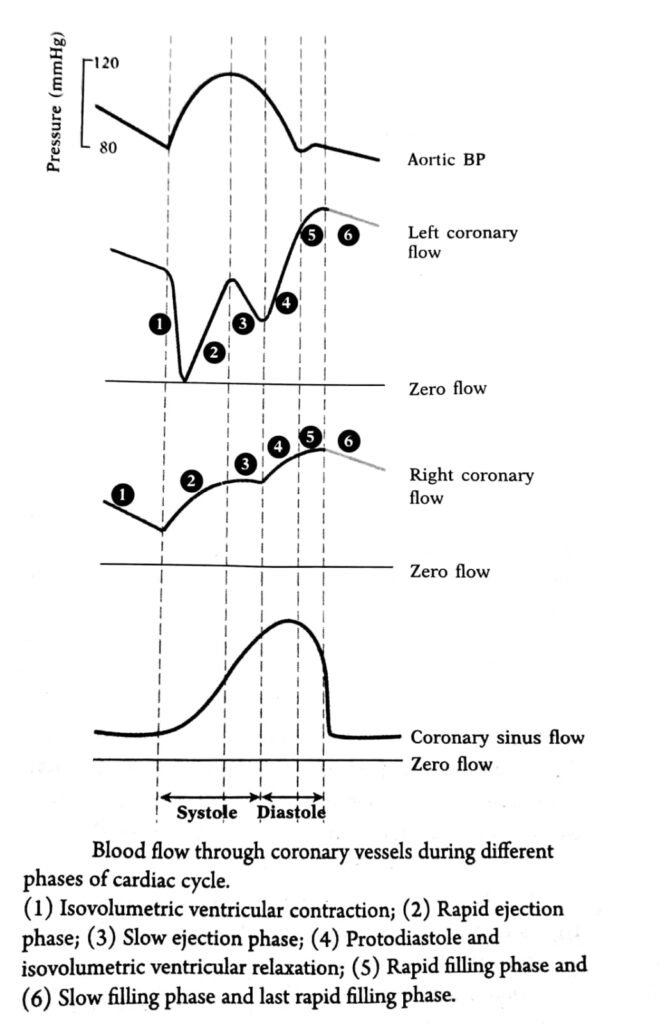
Describe the phasic changes in coronary circulation and its clinical importance. Give an account of regulation of coronary blood flow
PHASIC CORONARY FLOW
During isovolumetric contraction
• Ventricles contract without any change in the length of the muscle fiber.
• Blood is not leaving the chamber.
• Blood flow to LV muscle reduces to zero
During ejection
-Aortic pressure increases but the contracting ventricles are compressing the vessels,
-thus the flow is present but less.
During isovolumetric relaxation
• Ventricles are relaxing.
• Sharp increase in the coronary blood flow
• Maximum coronary blood flow During diastasis & late filling
• Aortic pressure decreases, so the coronary blood flow is less
Regulation of Coronary Blood Flow
Mechanisms involved:
1. Autoregulation
2. Neural regulation
3. Hormonal regulation
Autoregulation:
– Heart regulates its own blood flow. This is called as autoregulation
– Autoregulation is by two mechanisms – Myogenic & chemical
Myogenic: The contraction and relaxation of the vascular smooth muscle
adjust the coronary blood flow when the blood flow is altered
Chemical regulation:
1. Hypoxia
2. Other metabolites ( CO2, H+
, K+ & lactate)
3. Local vasodilators
Hypoxia: Increases coronary blood flow by causing vasodilatation
This is done by two mechanisms:
a. Direct effect:
Decreased myocardial oxygen
↓
Intracellular acidosis
↓
Less calcium binding
↓
Relaxation of vascular smooth muscle
↓
vasodilatation
↓
Increase in coronary blood flow
b. Trough adenosine: (Berne’s hypothesis)
in myocardial metabolism
↓
Hypoxia & adenosine (from ATP)
↓
Vasodilatation
↓
Increase in coronary blood flow
Other metabolites : ( CO2, H+
, K+ & lactate)
Decrease in coronary blood flow
↓
Accumulation of metabolites
↓
Vasodilatation
↓
Increase in coronary blood flow
Local vasodilators: (NO (EDRF), Prostacyclin & bradykinin)
Decrease in coronary blood flow
↓
Release of vasodilators by vascular endothelium
↓
Vasodilatation
↓
Increase in coronary blood flow
Neural regulation:
Sympathetic nervous system (nor-adrenergic fibers)
• Stimulation of the receptors → vasoconstriction →decrease in coronary blood
flow (direct effect)
• Stimulation of receptors → increase in heart rate & myocardial contractility →
accumulation of metabolites → vasodilatation → increase in coronary blood flow
(Indirect effect)
• Coronary vascular dilatation → Preservation of the supply to the heart.
parasympathetic nervous system
• Stimulation
— directly → vasodilatation.
— indirectly → vasoconstriction
Hormonal regulation:
1. Catecholamines: Same as that of sympathetic stimulation
2. Acetylcholine: Same as that of parasympathetic stimulation
3. Vasopressin: Vasoconsrtiction
4. Angiotensin: Vasoconstriction
5. Thyroxine: Increases metabolism → Hypoxia → vasodilatation → increase in
coronary blood flow
Clinical importance:-
1. Variation in CBF with heart rate. The duration of diastole is shortened to a much greater extent from 0.5 sec (at HR 72 bpm) to 0.14 sec at (HR 200 bpm). Therefore CBF also decreases.
2. Because there is no blood flow during systole in subendocardial portion of ‘LV’, therefore, this portion of ‘LV’ is more prone to ‘MI’ (Myocardial infarction).
3. In aortic stenosis: ‘LV’ pressure is further increased because the pressure in the ‘LV’ must be much greater than that in the aorta to eject blood, therefore, coronaries supplying the ‘LV’ are severely compressed during systole, hence leads to MI due to:
(i) Compression of coronaries, and
(ii) ‘LV’ has to do more work to expel the blood through the stenosed valves; this increases oxygen consumption of the ‘LV’.
4. In congestive cardiac failure (CCF), increase in venous pressure decreases aortic diastolic pressure. Thus effective coronary perfusion pressure falls and ‘CBF decreases.