Function of blood?
- Transport of oxygen and carbon dioxide
- Transport of nutrients and waste products
- Regulation of body temperature
- Maintenance of pH balance
- Protection against infection and diseases
- Clotting to prevent excessive bleeding
- Maintenance of fluid and electrolyte balance
Function of platelets?
- Platelets help in blood clotting.
- They release clotting factors to promote coagulation.
- They also help in wound healing and repair by releasing growth factors.
- Platelets play a role in inflammation and immunity by releasing cytokines and chemokines.
- They help maintain the integrity of blood vessels by releasing substances that promote vasoconstriction.
Blood clotting factors
- Factor I: Fibrinogen
- Factor II: Prothrombin
- Factor III: Tissue factor
- Factor IV: Calcium ions
- Factor V: Proaccelerin or labile factor
- Factor VI: Unassigned
- Factor VII: Stable factor or proconvertin
- Factor VIII: Antihemophilic factor or antihemophilic globulin
- Factor IX: Christmas factor or plasma thromboplastin component
- Factor X: Stuart-Prower factor or thrombokinase
- Factor XI: Plasma thromboplastin antecedent or antihemophilic factor C
- Factor XII: Hageman factor or glass factor
- Factor XIII: Fibrin-stabilizing factor.
Vitamin k dependent clotting factors
- Factor II (prothrombin)
- Factor VII (proconvertin)
- Factor IX (Christmas factor)
- Factor X (Stuart-Prower factor)
Factors stimulating Erythropoiesis
- Hypoxia
- Anemia
- Reduced oxygen-carrying capacity of blood
- Increased altitude
- Increased physical activity
- Endocrine factors (e.g. erythropoietin, thyroid hormone)
Features of pernicious anemia
- Caused by a deficiency of vitamin B12
- Due to the inability to absorb vitamin B12 from the digestive tract
- Results in decreased red blood cell production
- Symptoms include fatigue, weakness, pale skin, shortness of breath, and numbness or tingling in the hands and feet
what are the types of haemoglobin
There are several types of hemoglobin, including:
Hemoglobin A (HbA): The most common type of hemoglobin found in adults, consisting of two alpha chains and two beta chains.
Hemoglobin A2 (HbA2): A minor form of hemoglobin, composed of two alpha and two delta chains.
Hemoglobin F (HbF): The predominant hemoglobin found in fetuses, consisting of two alpha and two gamma chains.
Hemoglobin S (HbS): An abnormal form of hemoglobin that causes sickle cell disease, characterized by the presence of a mutated beta chain.
Hemoglobin C (HbC): An abnormal form of hemoglobin caused by a mutation in the beta chain.
write short note on Erythropoiesis
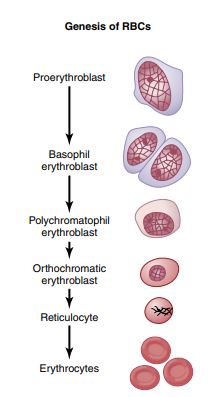
#characteristic features of Erythropoiesis –
- Reduction in cell size
- Cytoplasm increase in amount. and nucleus decrease in size
- Staining reaction of cytoplasm changes from deep basophilic to polychromatophilic (acidophilic + basophilic & finally to orthochromatic, due to gradual reduction in RNA amount.
- Disappearance of Nucleus and Nucleoli.
- [NOTE] : The rate of erythropoiesis is measured by reticulocytes count. Normally <1% of the old RBC are replaced by new reticulocyte on any given day. Thus reticulocytes counts for about 0.5-1% of all RBC in normal blood sample.
1. Erythropoietin a hormone secreted by kidneys
– Stimulates the bone marrow tissue to produce more RBCs.
2. Hypoxia: Lack of O2 is the main condition which stimulates erythropoietin secretion.
Lack of O2 (Hypoxia)
↓
Kidneys
↓
Erythropoietin
↓
Red Bone marrow
↓
Increased RBC Production
↓
Restoration of O2 Supply
3. Nutrients:
a) Proteins for synthesis of Hb.
b) Minerals:
i) Iron : for synthesis of heme part of Hb.
ii) Copper: for synthesis of Hb.
4. Vitamins:
a) Vitamins B12 & Folic Acid: Required for synthesis of DNA. These factors are called maturation factors.
b) Vitamin C is also required.
5. Hormones:
Thyroxine
Glucocorticoids
Testosterone
Growth hormone
Thus:- stimulates erythropoietin increases RBC production
Normal Count of RBC:
– Male 5-6 million/cu mm of blood
– Female 4.5 – 5.5 millions/cu mm of blood.
#FACTORS AFFECTING ERYTHROPOIESIS:
FACTORS AFFECTING ERYTHROPOIETIN PRODUCTION:
INCREASE IN:
1. Hypoxia due to:
a) Haemorrhage →Decreases blood volume
b). High altitude:- Decrease O₂ quantity in air
c). Prolonged cardiac failure- decrease tissue blood flow
d).Lung disease-decrease tissue blood flow
2. Vasoconstrictor agents:
a).Epinephrine
b). Non Epinephrine
3. Hormones:
a).Thyroid hormone→ thyrotoxicosis- Polycythemia
→ Myxedema- Anaemia
b). Androgens → Stimulates exythropoiesis & potentiate the action of erythropoietin
DECREASE IN:
1).Oestrogen Depresses the erythropoietic response to hypoxia.: Female RBC count is less compared to males..
2).Chronic renal disease.
3).Cirrhosis of liver
4).Protein deficiency.
What is Erythroblastosis fetalis
Erythroblastosis fetalis, also known as hemolytic disease of the newborn, is a condition in which red blood cells of a developing fetus are destroyed by antibodies produced by the mother’s immune system. This condition occurs when the mother has Rh-negative blood and the fetus has Rh-positive blood. During delivery or any other event that may cause mixing of the blood, the mother’s immune system is exposed to the Rh-positive blood and produces antibodies against it.
These antibodies can cross the placenta and attack the fetus’s red blood cells, leading to anemia and other complications. Symptoms of erythroblastosis fetalis can range from mild to severe, including jaundice, anemia, brain damage, and even death.
Fortunately, erythroblastosis fetalis can be prevented with the use of Rh immunoglobulin, a medication that can prevent the mother’s immune system from producing antibodies against the Rh-positive blood.
Describe anemia and its types add a short note on a) iron deficiency anemia b) pernicious anemia
Defination-Anaemia is a clinical condition in which the carrying capacity of blood is reduced. It is characterized by reduction in the number of RBCs less than 4 million/μL or their content of haemoglobin less than 12 gm/dL or both.
Grading:-
1.Mild Anaemia : Haemoglobin 8-12 gm/dL
2.Moderate Anaemia: Haemoglobin 5-8 gm/dL
3.Severe Anaemia : Haemoglobin less than 5 gm/dL
Classification
(A) Etiological or Whitby’s Classification. This is based on the cause of anaemia.
- Haemorrhagic – Anaemia due to blood loss
- Dietary deficiencies due to iron, vitamins and proteins etc
- Dyshaemopoiesis or abnormal haemopoiesis resulting in aplastic anaemia.
- Hemolytic anaemia- anaemia is due to excessive destruction of RBC
(B) Morphological or wintrobe’s classification
- Normocytic-
(a) normocytic normochromic
(b) normocytic hypochromic - Macrocytic
(a) macrocytic normochromic
(b) macrocytic hypochromic - Microcytic
(a) microcytic normochromic
(b) microcytic hypochromic
What is Iron deficiency anaemia
Iron Deficiency Anaemia
This is the most frequently seen anemia and is due to iron deficiency. The erythrocytes are smaller and pale, hence the name microcytic and hypochromic anaemia. Iron is required for haem synthesis. It is mainly absorbed from the duodenum.
Causes:
(1) Inadequate intake,
(2) Increased loss
- i. Acute haemorrhage as in: accidents
- ii. Chronic haemorrhage as in:
a) Excess menstruation
b) Bleeding ulcers
c) Piles, etc.
- iii. Increased demand as in:
a) Pregnancy
b) Lactating mother
c) Growing children - iv. Poor absorption due to disease of stomach and duodenum
- v. Copper difficiency also causes as it is required for iron absorption.
Features
1. Type of anaemia: Microcytic hypochromic anaemia
2 Blood changes
- a) RBC are smaller (<6.2µ ) and pale
- b) RBC count is less
- c) Hb content /100 mL. is less
- d) MCV, MCH and MCHC are less than normal
- e) Platelet count is increased
- f) Low serum and urine iron levels
3. Bone marrow: Bone marrow is normoblastic and hyper- plastic
4. Cardiorespiratory changes
- a) Breathlessness and palpitation on exertion
- b) Repeated lung infections due to decreased immunity
5. Nervous system: Increased irritability and loss of concentration.
6. Nails: Nails become dry, soft and spoon shaped.
7. Tongue: glossitis, red in colour, atrophy of tongue papillae.
Management: Administration of ferrous iron either orally or intramuscularly corrects the anaemia.
What is megaloblastic anaemia
Megaloblastic Anaemia
It is due to deficiency of maturation factors B12 and folic acid. Both these vitamins are required for synthesis of DNA. Vita min B12 acts as a co-enzyme and is absorbed from the ileum. Intrinsic factor produced by the gastric parietal cell is neces sary for the absorption of B12, Megaloblastic anaemia due to specific deficiency of the B12 is called pernicious anaemia as it is associated with severe neurological disorder.
B12 Deficiency
Causes:
1. Inadequate intake,
2. Intrinsic factor deficiency.
3. Defective absorption.
B12, deficiency affects both the haemopoietic system and the nervous system and is mainly due to defective absorption.
Features
1. Type of anaemia: Macrocytic normochromic anaemia
2. Blood changes
a) RBC are larger and normochromic.
b) RBC, WBC and platelet counts decrease.
c) Hb content per 100 mL is reduced.
d) Shortened lifespan: The large RBC (8.2 µ) as they pass through the capillary are prone to get damaged, there by the shortened life span.
e) MCV and MCH increase while MCHC remains normal.
3. Bone marrow changes
- a) Bone marrow shows hyperactivity due to anaemic hypoxia.
- b) Megaloblasts, large proerythoblasts accumulate in large numbers.
b) Glossitis (inflammation of tongue).
5. Changes in nervous system(**)
- a) Subacute combined degeneration of spinal cord in which both sensory and motor tracts are affected.
- b) Peripheral neuropathy is present.
- c) Loss of memory, depression and ataxia are present.
- d) Hyper reflexia and paralysis.
Folic Acid Deficiency
Causes:
1. Inadequate intake
2 Increased demand
3. Poor absorption as in sprue
4. Persons on anti-metabolite treatment
(note)-In folic acid deficiency the same features are seen except neurological symptoms.
Management: Vitamin B12 therapy restores both haemato-logical and neurological function. In pernicious anaemia, B12 should be given parenterally along with large oral dose. Administration of folic acid restores the haematological function but not neurological function. Neurological complications may worsen with folic acid treatment alone although its deficiency does not itself cause neurological disturbances. Hence both B12 and folic acid are given together.
short note on pernecious anaemia
Pernicious anemia is a type of megaloblastic anemia that occurs when the body cannot absorb enough vitamin B12 from the gastrointestinal tract. This may be due to the lack of intrinsic factor, a protein produced by the stomach lining that is required for vitamin B12 absorption. Pernicious anemia can also occur due to autoimmune destruction of parietal cells in the stomach, which produce intrinsic factor.
The symptoms of pernicious anemia include fatigue, weakness, shortness of breath, pallor, and neurological symptoms such as numbness and tingling in the hands and feet, difficulty walking, and memory problems. Treatment typically involves regular injections of vitamin B12, which can help to alleviate the symptoms of the condition and prevent complications.
If left untreated, pernicious anemia can lead to serious complications such as nerve damage, cognitive impairment, and heart failure. Therefore, it is important to seek medical attention if you suspect you may have pernicious anemia.
Treatment of pernicious anemia involves regular injections of vitamin B12. In some cases, oral supplements may be effective, but injections are typically more effective because they bypass the need for intrinsic factor in the digestive tract. With proper treatment, the symptoms of pernicious anemia can be managed effectively, but if left untreated, it can lead to serious and potentially life-threatening complications.
Describe the ABO and Rh blood groups, Clinical significance. What is Cross matching
The ABO and Rh blood groups are two important systems used to classify blood types based on the presence or absence of certain antigens and antibodies.
ABO Blood Group System:
The ABO system includes four blood types: A, B, AB, and O.
The blood types are determined by the presence or absence of two antigens: antigen A and antigen B.
- People with blood type A have antigen A on their red blood cells,
- people with blood type B have antigen B,
- people with blood type AB have both antigens, and
- people with blood type O have neither antigen.
Rh Blood Group System:
The Rh system refers to the presence or absence of a specific antigen, the Rh factor, on red blood cells. People who have the antigen are Rh positive (Rh+), and those who do not are Rh negative (Rh-). Rh incompatibility can occur during pregnancy when the mother is Rh- and the fetus is Rh+. This can result in hemolytic disease of the newborn, where the mother’s antibodies attack and destroy the fetus’s red blood cells.
Cross matching:
Cross matching is a laboratory test that is performed prior to a blood transfusion to ensure compatibility between the donor’s and recipient’s blood. The test involves mixing a small amount of the donor’s blood with the recipient’s blood and observing for any reactions. If there is no reaction, the blood is considered compatible, and the transfusion can proceed. If there is a reaction, the transfusion cannot proceed as it could lead to a transfusion reaction in the recipient. Cross matching is important to prevent transfusion reactions such as hemolysis, fever, chills, and anaphylaxis.
Clinical Significance:
The ABO and Rh blood groups are important in clinical settings, particularly for blood transfusions and in cases of hemolytic disease of the newborn. Knowing a person’s blood type helps ensure that they receive the correct blood type during a transfusion to prevent transfusion reactions. In addition, Rh incompatibility can lead to severe health consequences during pregnancy and childbirth, making it important to identify and manage Rh-negative mothers during prenatal care.
Why blood does not clot in circulation
1. Endothelial factors:
(i) Smoothness of endothelial lining prevents platelets adhesion and extension of clot into blood vessel.
(ii) Negatively charged particles (such as glycocalyx, a mucopolysacoharide) present over endothelial lining, repel the clotting factors i.e. protein anions, thereby prevent clotting.
2. Velocity of circulation; if decreases leads to clotting.
3. Presence of natural anticoagulants in the blood e.g. heparin and protein ‘C
4.Simultaneous activation of fibrinolytic system along with clotting mechanism .
5. In the event of spontaneous clot formation, liver removes the activated clotting factors from the circulation.
Thanks very much for the noble work done my you it’s really helpful
Novyny
Very helpful sir
Thank you sir
It’s really very helpful