Discuss the long term regulation of Arterial blood pressure.
1. Renal body fluid mechanism
2. Renin-Angiotensin mechanism
3. Hormones – Aldosterone & ADH
Increase in BP
↓
Increase in renal blood flow
↓
Increase in GF
↓
Increase in urine formation
↓
Decrease in ECF volume
↓
Decrease in BP
(Restoration of BP)
Decrease in BP
↓
Decrease in renal blood flow
↓
Decrease in GFR
↓
Decrease in urine formation
↓
Increase in ECF volume
↓
Increase in BP
(Restoration of BP)
¯Renin – Angiotensin Mechanism:
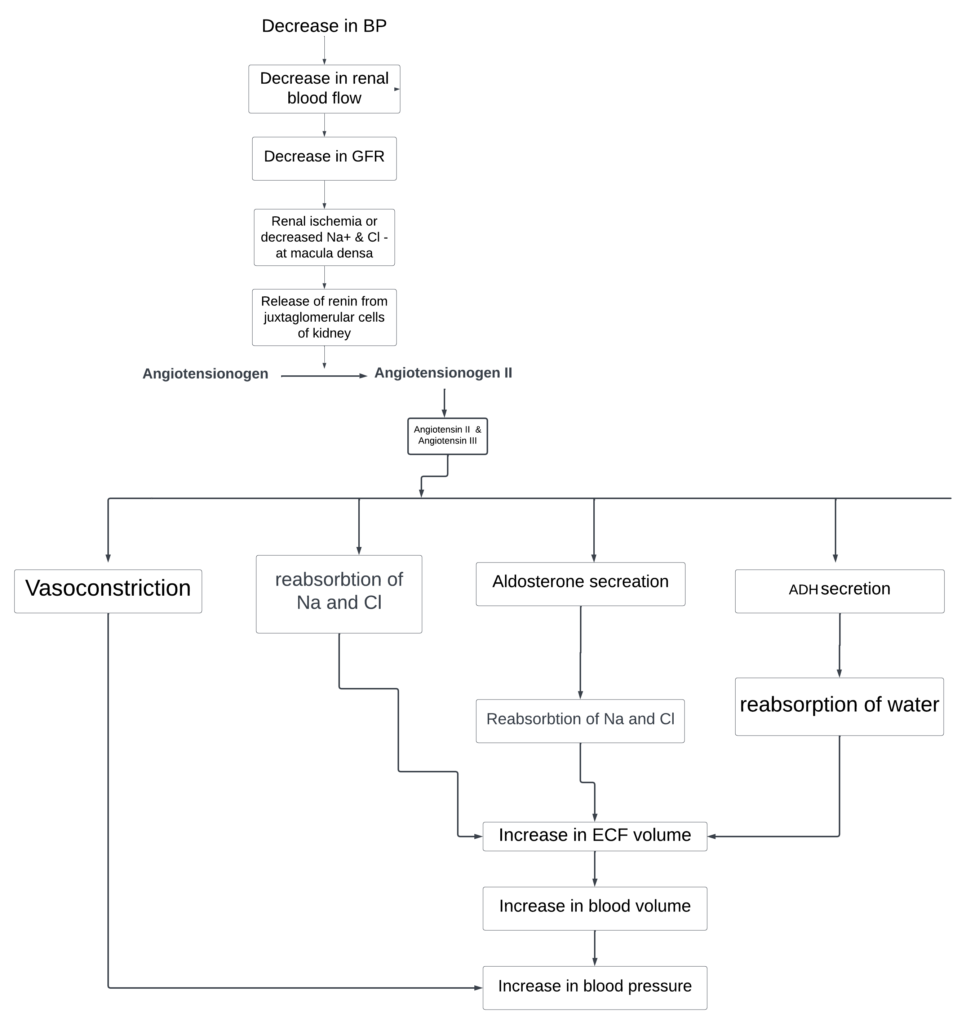
Hormones Regulating Blood Pressure:
Aldosterone: Secreted from adrenal cortex in response to decrease in ECF volume. Increases the reabsorption of Na+ & Cl in kidney tubules. This causes increase in ECF volume and blood pressure
ADH: Secreted from posterior pituitary. Increases water reabsorption from kidney →increase in ECF volume and blood pressure
ANP: Secreted from atrial myocardium in response to increase in ECF volume →facilitates Na+, Cl-& H2O excretion into urine → decrease in ECF volume & blood pressure
Describe the short-term regulation of Arterial blood pressure
Short – Term or Rapid Acting Mechanisms
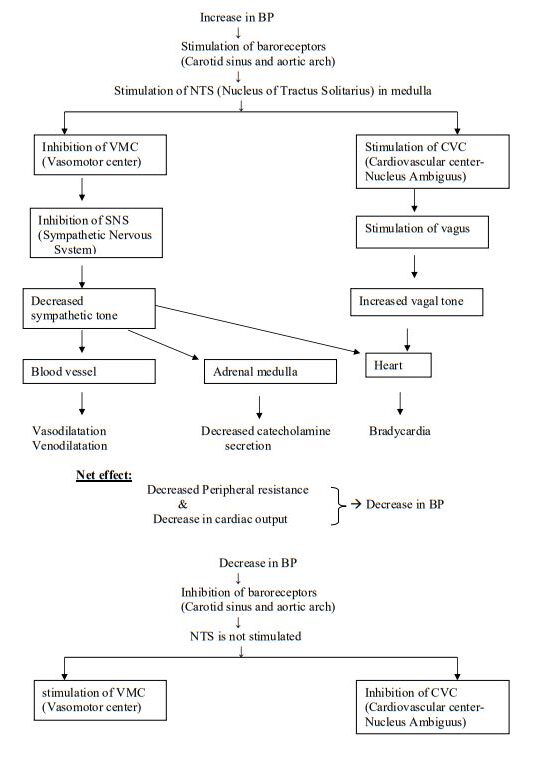
1. Baroreceptor reflex
2. Chemoreceptor reflex
3. Cushing reflex
4. Capillary fluid shift
5. Hormones
Baroreceptor reflex:
– Also called as “Marey’s reflex” or “Sino-Aortic reflex”
– Initiated by increase in blood pressure
– Receptors are mechanoreceptors which respond to stretch in blood vessel wall
– Receptors are called “Baroreceptors”. They are present in the carotid sinus and aortic arch
– This mechanism can correct 2/3rd of fall in BP
– The working range of BP is 60-200 mm Hg
CNS ischemic response:
– This mechanism occurs due to ischaemia of brain
– This may result due to severe fall in BP below 40 mmHg
– If this response is specifically due to increase in intracranial pressure, it is called as “Cushing reflex”
– The response is called “last ditch effort” as it tries to prevent the death of a person
– The working range for this mechanism is 15-50 mm Hg
– It can correct 90% of the fall in BP
Decrease in BP (below 40 mm hg)
↓
Decreased blood flow to the brain
↓
Ischemia of brain
↓
Stimulation of VMC
(Vasomotor center)
↓
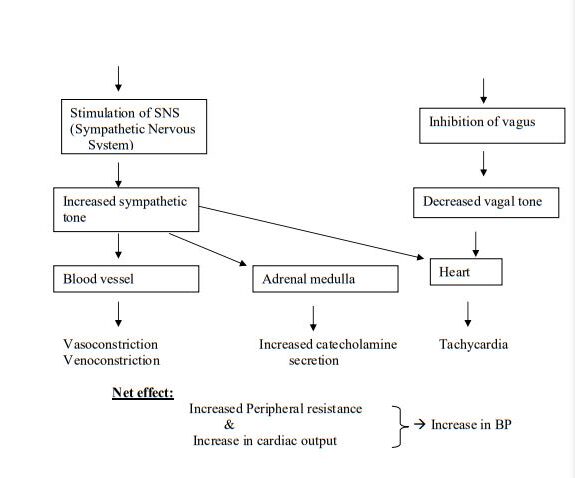
Stimulation of SNS
(Sympathetic Nervous System)
↓
Increased sympathetic tone
↓
Blood vessel
↓
Vasoconstriction
↓
Increase in BP
Chemoreceptor Reflex:
– Receptors respond to chemicals. So called as chemoreceptors
– Two types of receptors – peripheral & central chemoreceptors
– Peripheral chemoreceptors – Carotid bodies & Aortic bodies
– Stimuli for receptors : Hypoxia, Hypercapnia & Acidosis
Decrease in BP (<40 mm Hg)
↓
Cerebral hypoxia, hypercapnia & acidosis
↓
Stimulation of VMC (Vasomotor center)
↓
Stimulation of SNS
(Sympathetic Nervous System)
↓
Increased sympathetic tone
↓
Blood vessel
↓
Vasoconstriction
Capillary Fluid Shift Mechanism:

Hormones:
1. Catecholamines: Fall in BP → release of catecholamines (epinephrine &
norepinephrine) from adrenal medulla → Vasoconstriction & increase in cardiac output→ increase in BP
2. ADH: In large amounts ADH causes vasoconstriction → increase in BP
3. Glucocorticoids: Cortisol and corticosterone sensitize the vascular smooth muscle to the action of catecholamines (permissive role)
4. Nitric oxide (Endothelium Derived Relaxing factor) :released by endothelium and acts locally causing vasodilatation
What is vasomotor center? What are its inputs and functions
Vasomotor Centre (VMC)
(i) The ventrolateral region of medulla contains glutaminergic neurons which exert excitatory effects on spinal sympathetic neurons. These neurons in medulla show inherent tonic activity i.e. they discharge rhythmically in a tonic fashion to excite sympathetic pre-ganglionic neurons in the intermediolateral grey column of the spinal cord Thus, sympathetic activity increases producing pressor effects on the CVS which includes:
(a) increase in heart rate,
(b) increase in stroke volume,
(c) increase in systemic BP due to increase arteriolar constriction, and
(d) venoconstriction which decreases blood stored in venous reservoir and increases venous return.
Therefore, the area in the ventrolateral region of medulla where these neurons are located is called pressor area

(ii) Near medial and distal parts of fourth ventricle in medulla certain groups of neurons are located. Stimulation of these neurons decreases sympathetic activity by inhibiting the tonically discharging impulses of the ‘pressor” area neurons producing depressor effects on the CVS. The effects include:
(a) decrease in heart rate,
(b) decrease in stroke volume,
(c) decrease in systemic blood pressure due to vasodilatation, and
(d) venodilatation which increases storage of blood in venous reservoirs and decreases venous return.
Thus the area in the medulla where these neurons are located is called depressor area.
(iii) In the intermediate region of the upper medulla, the ‘depressor’ and ‘pressor’ areas overlap i.e. there is no clear anatomical separation between two areas. Thus, the two areas together constitute medullary cardio-vascular centre. However, these neurons exert predominantly excitatory effect on thoraco lumbar sympathetic neurons in the spinal cord. Therefore, the term vasomotor centre (VMC) is more commonly used.
Note : VMC can thus produce either:
(i) increase in sympathetic activity due to increase activity of pressor area; or
(ii) decrease in sympathetic activity due to increase activity of depressor area which in turn inhibits the pressor area.