Explain the counter current mechanism in the concentration of urine
COUNTERCURRET MECHANISM OF CONCENTRATING THE URINE
Normal osmolarity of urine: 300 mosm/lt
Osmolarity of diluted urine: Upto 50mosm/lt
Osmolarity of concentrated urine: Upto 1200mosm/lt
Requirements for concentrating the urine:
1. ADH
2. Hyperosmolar medullary interstitium
Factors contributing to hyperosmolarity of medullary interstitium:
1. Countercurrent system
2. Reabsorption at DCT & CD
3. Urea recirculation
1. Countercurrent system: A system in which the inflow runs in parallel, in opposite direction & in close proximity to the outflow
Components of countercurrent system in kidney:
a) Loop of Henle (contercurrent multiplier)
b) Vasarecta (countercurrent exchanger)
Role of Loop of Henle as countercurret multiplier in countercurrent mechanism:
To generate osmotic gradient & hyperosmolarity of medullary interstitium
Mechanism –
– Diffusion of water out of thin descending limb of LOH (This makes the fluid in the tip of the loop to become more concentrated than the surrounding interstitum)
– Passive reabsorption of solutes from the hypertonic fluid in the tin ascending limb (This helps in multiplication of interstitial osmolarity)
– Active reabsorption of sodium & chloride in the thick ascending limb of Loop of Henle (This helps in building up of a higher interstitial osmolarity)
Role of vasa recta as countercurrent exchanger in countercurrent mechanism:
To maintain the osmotic gradient & hyperosmolarity of medullary interstitium
Mechanism –
Descending limb of vasa recta :
– Solutes diffuse into the lumen
– Water diffuses out
– The osmolarity of blood increases from 300 milliosmoles to 1200 milliosmoles towards the tip of vasa recta
Ascending limb of vasa recta:
– Solutes move out
– Water diffuses in
– The osmolarity of the blood decreases from 1200 milliosmoles to 300 milliosmoles from the tip upwards So the solutes are exchanged for water between the ascending and the descending limbs of vasa recta. This maintains the hypertonicity of medulla.
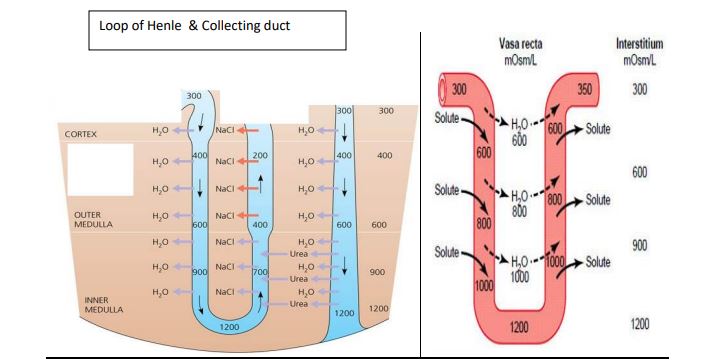
2. Reabsorption in the DCT & Collecting duct:
• Sodium ions are actively absorbed from distal tubule and collecting duct under the
influence of aldosterone.
• Sodium ions are accompanied passively by chloride ions.
• This also increases the medullary osmotic gradient
3. Urea recirculation:
• Large amounts of urea is reabsorbed in the medullary collecting duct.
• The urea which moves into the interstitium is secreted in to the descending &
ascending limb of LOH.
Loop of Henle & Collecting duct
• Again it is reabsorbed in the medullary collecting duct.
• This recirculation of urea before it is excreted in the urine helps to generate medullary
osmotic gradient
• Urea recirculation contributes 40% to hyperosmolarity of medullary interstitium
ADH: Increases urea reabsorption (This increases the interstitial osmolarity)
Increases water reabsorption (This makes the urine concentrated)
Renal blood flow: Slow rate of blood flow through the medulla causes retention of sodium in
the medullary interstitium
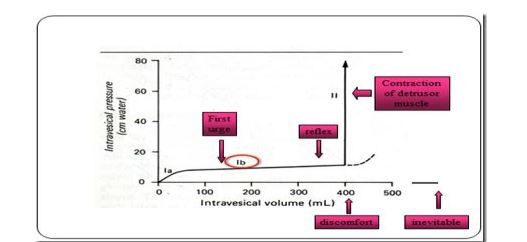
Cystometrogram and its significance
Definition: Cystometrogram is a graphical record showing the relationship between the intravesicular volume and pressure of urine in the urinary bladder
Phases of normal cystometrogram:
a) Phase Ia
b) Phase Ib
c) Phase II
a) Phase Ia : Initial rise in intravesicular pressure
– Rise in intravesicular pressure when about 50 ml of urine is collected in the bladder
Basis: Filling of bladder with urine → stretching of bladder wall → contraction of muscles of bladder wall → increase in pressure from 0-10 cm of H2O
b) Phase Ib: (Pleateau phase)
– No rise in the pressure (remains at 10 cm of H2O) till the bladder volume is 400 ml
Basis: Can be explained by Laplace Law (Laplace law: P = 2T / R where ‘P’ is the pressure, ‘T’ is the tension in the wall & ‘R’ is the radius of the bladder
Explanation:
Urine accumulation → increase in tension of the bladder wall, but there is increase in radius of the bladder too (called as plasticity of the smooth muscle). The effects of these two factors get neutralized & the pressure remains same.
c) Phase II: Steep rise in intravesicular pressure:
– Starts beyond 400 ml
– Tension of wall increases due to contraction of detrussor muscle, but
radius is not increased. So, the pressure increases (20 cm to 40 cm of
H2O)
-This stimulates voiding sensation (triggering the micturition reflex)
Describe the mechanism of urine formation
Every day kidney produces 1 – 2 liters of urine.
The mechanism of urine formation involves three processes:
a) Glomerular filtration
b) Tubular reabsorption
c) Tubular secretion
a) Glomerular filtration:
– Process by which the fluid along with the substances dissolved in it passes from the glomerular capillaries in to the Bowman’s capsule is called glomerular filtration
– Blood cells and plasma proteins are not filtered
– Filtration occurs through filtering membrane which is made up of 3 layers – Fenestrated
capillary endothelium, basement membrane & podocytes (epithelial cells of Bowman’s capsule) with filtration slits
– The fluid which gets collected in the capsule is called filtrate
– The amount of filtrate formed per minute (GFR – Glomerular Filtration Rate) is 125ml.
– This is mainly determined by net filtration pressure which depends upon the Starling forces
acting across the filtering membrane – Glomerular capillary hydrostatic & colloidal osmotic pressure,
Bowman’s capsule hydrostatic pressure
b) Tubular reabsorption:
– Passage of water and solutes from the filtered fluid in the kidney tubule into the blood is called tubular reabsorption
– Solutes which are reabsorbed are nutrients (glucose & aminoacids), electrolytes (sodium, potassium & chloride) & ions such as bicarbonates.
– The modes of transport are both passive & active transport mechanisms
Reabsorption At Proximal Convoluted Tubule:
– Majority of reabsorption takes place at PCT as the surface area is increased due to presence of brush border microvilli
– 65% of filtered water, sodium, chloride, potassium and other solutes
– 100% of glucose and amino acids
– Sodium is reabsorbed by secondary active transport along with substances like glucose and amino acids
– This is followed by osmosis of water into the blood. The reabsorption of water at PCT is called obligatory reabsorption of water
– The reabsorption of water and sodium are exactly proportional. So the fluid which leaves the PCT is isotonic
Reabsorption At Loop of Henle:
– Loop of Henle consists of three segments – Descending limb, thin ascending limb & thick ascending limb
– About 20% of filtered sodium and chloride, 15% of filtered water and cations such as K+ , Ca2+ and Mg2+ are reabsorbed in the Loop of Henle
– In the descending limb, water absorption occurs passively because of hypertonic interstitial fluid in this part
– The thin ascending limb is impermeable to water. Limited passive absorption of sodium and chloride occurs
– Thick ascending limb is impermeable to water. 20% of filtered sodium and chloride and other cations are reabsorbed here by the following mechanisms:
– Sodium, potassium – 2 chloride symporter mediated active transport of sodium
– Na+ – H + antiporter mediated active reabsorption
– Paracellular passive reabsorption of Na+, K+, Ca2+ & Mg+
– Sodium reabsorbed here is the main driving force behind the countercurrent multiplier system which concentrates sodium and urea in medullary interstitium
– As the reabsorption of solutes is not followed by water reabsorption, the fluid that leaves this segment is hypotonic compared to plasma. Hence this segment is called diluting segment
Reabsorption At Distal Convoluted Tubule (DCT) & Collecting Duct (CD)
– Approximately 7% of filtered NaCl & 8 to 17% of water is resbsorbed
– Late DCT & CD have two cell types – “P” (Principal) cells & “I” (Intercalated) cells
– Principal cells reabsorb Na+ , Cl- & H2O
-Intercalated cells reabsorb K+
– H2O reabsorption by principal cells is influenced by the hormone ‘ADH’-Anti Diuretic Hormone. The reabsorption of water at this segment is called facultative reabsorption of water.
– Na+ reabsorption by principal cells is influenced by the hormone aldosterone which is secreted from the adrenal cortex
c)Tubular Secretion:
The substances which escape filtration are transported from peritubular capillary in to the tubular fluid.
This transport is called tubular secretion.
Substances secreted:
- – H+ ions, K+, NH3-
- – Drugs
- – Pencillin
- – Creatinine
Secretion at PCT:
– Organic anions & cations
– Exogenous organic compounds
– Certain drugs
– H+ & NH3- are secreted. H+ is secreted in exchange with Na+ absorption. This is mainly utilized for the absorption of HCO3
Secretion at DCT & CD:
– K+ secretion by principal cells takes place. This is increased by hormone aldosterone
– H+ & NH3- are secreted. H+ secretion by intercalated cells is mainly responsible for acidification of urine.
Write short note on micturation reflex
Definition: The periodic complete voluntary emptying of the bladder is called micturition
Events involved:
– Micturition is basically a spinal reflex
– Influenced by higher centers
a) Micturition reflex
b) Voluntary control of micturition
c) Role of other muscles in micturition
a) Micturition reflex:
Stimulus: Filling of bladder by 300 to 400 ml of urineReceptors: Stretch receptors in the detrussor muscle
Afferent: Sensory fibers in pelvic nerve
Center: S2, S3 & S4 of sacral segments
Efferent: Motor fibers in pelvic nerve
Effector organ: Detrussor muscle of urinary bladder & internal urethral sphincter
Response: Contraction of detrussor muscle of the bladder & relaxation of the urethral Sphincter
(Excitation of parasympathetic afferent fibers causes inhibition of pudendal nerve → relaxation of external urethral sphincter)
b) Voluntary control of micturition: (Role of supraspinal centers)
Supraspinal centers involvedPons – Facilitate
Mid brain – Inhibits
Posterior hypothalamus – Facilitate
Limbic system — Facilitate
Basal ganglia – Inhibits
Cerebral cortex – Inhibits
c) Role of other muscles:
Perineal & abdominal muscles help the emptying of bladderAcidification of urine
– Normally the urine is acidic with a pH range from 4.5 to 6.0.
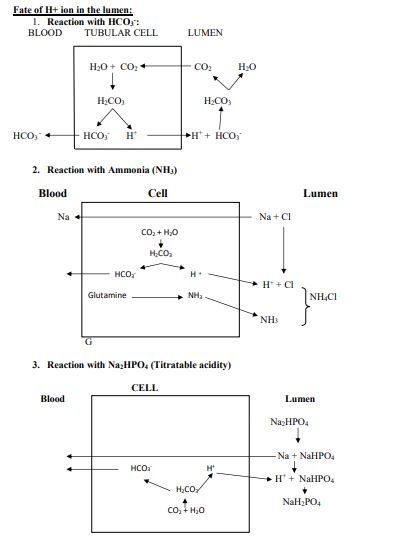
– Acidification of urine is brought about by H+
secretion in to the tubular fluid
– H+ secretion takes place throughout nephron.
– H+ secreted at PCT & LH is utilized for absorption of HCO3-. Does not contribute to acidification of urine.
– H+ secreted in small amounts in the DCT & CD is responsible for the acidification of urine